Latest Blog Articles
Behavioral and Social Research in Parasitology
Behavioral and Social Research in Parasitology: Addressing Socioeconomic Factors and Implementing Behavioral Interventions
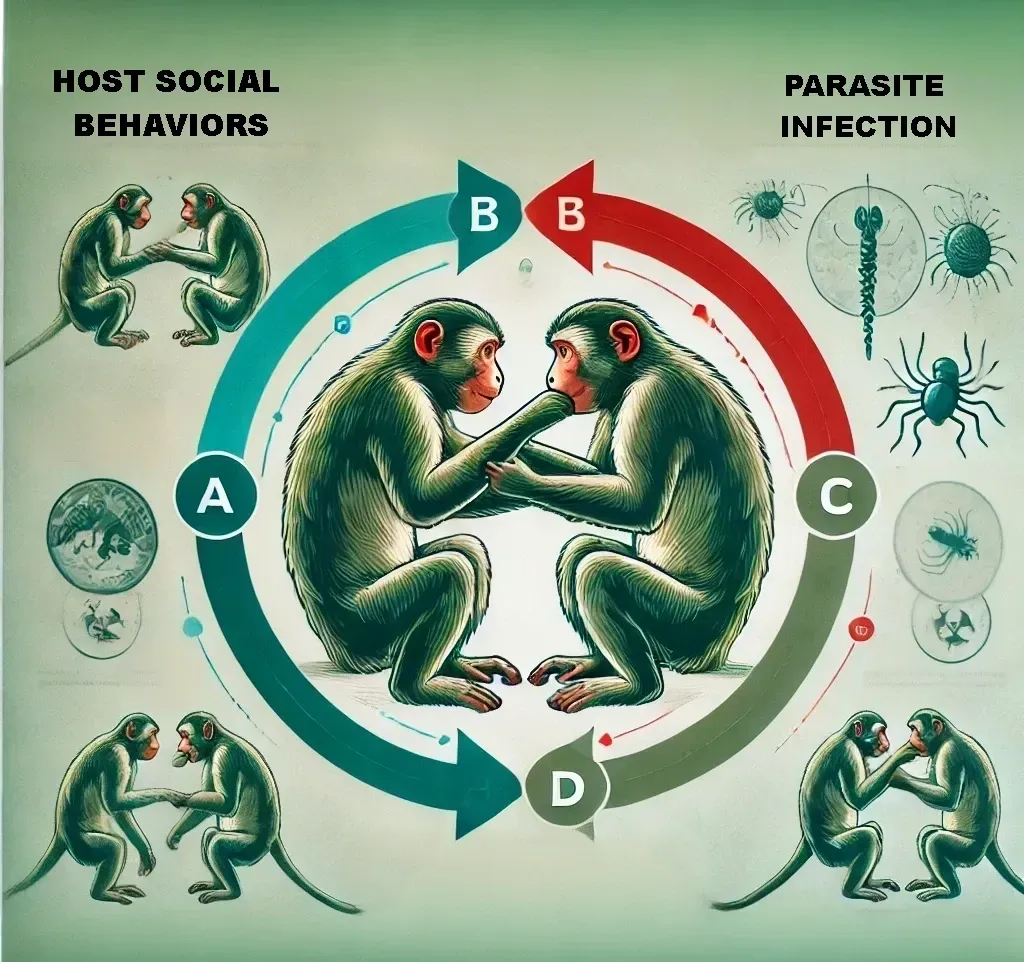
Parasitic diseases remain a significant global health challenge, disproportionately affecting marginalized and economically disadvantaged populations. As parasitology research evolves, there is an increasing recognition of the importance of behavioral and social factors in the transmission and impact of parasitic infections. Understanding and addressing these factors can lead to more effective control and prevention strategies. This post delves into the critical areas of behavioral and social research in parasitology, with a focus on socioeconomic factors and behavioral interventions.
Socioeconomic Factors: Understanding the Root Causes
Socioeconomic factors play a pivotal role in the prevalence and impact of parasitic diseases. These factors include income level, education, employment status, housing conditions, and access to healthcare. Research has shown that individuals and communities with lower socioeconomic status are more vulnerable to parasitic infections due to a combination of environmental, behavioral, and systemic factors.
Income and Poverty:
Living Conditions: Poor communities often lack adequate sanitation and clean water, creating environments where parasites thrive. For instance, helminth infections like hookworm and schistosomiasis are commonly associated with areas lacking proper sanitation.
Access to Healthcare: Low-income individuals frequently face barriers to accessing healthcare, including the cost of medical services, lack of transportation, and limited availability of healthcare facilities. This delays diagnosis and treatment, exacerbating the impact of parasitic diseases.
Education:
Awareness and Prevention: Education level is closely linked to health literacy. Individuals with limited education may not be aware of how parasitic diseases are transmitted or how to prevent them. Educational interventions can significantly improve knowledge and practices related to disease prevention.
Health-Seeking Behavior: Education also influences health-seeking behavior. Those with higher education levels are more likely to seek medical help promptly and adhere to treatment regimens.
Employment and Occupational Hazards:
Exposure Risks: Certain occupations expose workers to higher risks of parasitic infections. Agricultural workers, for example, are at increased risk of contracting parasitic diseases such as malaria and schistosomiasis due to exposure to water and soil contaminated with parasites.
Economic Stability: Employment status affects economic stability, which in turn influences the ability to afford preventive measures, such as bed nets for malaria or clean water for preventing waterborne parasites.
Housing and Urbanization:
Overcrowded Living Conditions: Overcrowding in urban slums can facilitate the spread of parasitic diseases. Inadequate housing and lack of infrastructure contribute to the persistence of vectors and pathogens.
Rural vs. Urban Divide: Rural areas often lack the infrastructure and healthcare resources available in urban settings, leading to higher rates of parasitic infections in these regions.
Addressing socioeconomic disparities requires a multifaceted approach that includes improving living conditions, enhancing access to education, and ensuring equitable healthcare services. By tackling these root causes, we can reduce the burden of parasitic diseases on vulnerable populations.
Behavioral Interventions: Changing Practices to Prevent Infection
Behavioral interventions aim to change individual and community practices to reduce the risk of parasitic infections. These interventions are based on an understanding of the cultural, social, and behavioral contexts in which people live. Effective behavioral interventions can lead to sustained improvements in health outcomes by promoting practices that prevent infection and transmission.
Health Education Campaigns:
Community Awareness: Health education campaigns tailored to specific communities can raise awareness about the modes of transmission and prevention of parasitic diseases. For example, educating communities about the importance of using latrines can reduce open defecation and soil-transmitted helminth infections.
School-Based Programs: Implementing educational programs in schools can instill healthy habits in children, such as handwashing and proper sanitation, which they can carry into adulthood.
Behavioral Change Communication (BCC):
Tailored Messaging: BCC strategies involve crafting messages that resonate with the target audience's values and beliefs. For instance, using culturally relevant storytelling to explain the benefits of using insecticide-treated bed nets can encourage their use to prevent malaria.
Mass Media Campaigns: Utilizing radio, television, and social media platforms to disseminate information can reach a broader audience and reinforce positive health behaviors.
Community Engagement and Participation:
Empowering Communities: Involving communities in the design and implementation of intervention programs ensures that they are culturally appropriate and accepted. Community-led initiatives, such as forming local health committees, can sustain long-term behavioral changes.
Peer Educators: Training community members as peer educators can enhance the credibility and effectiveness of health messages. Peer educators can provide ongoing support and reinforcement of healthy practices.
Environmental Interventions:
Improving Sanitation: Environmental interventions that improve sanitation infrastructure, such as building latrines and providing access to clean water, are crucial in reducing the transmission of parasitic diseases.
Vector Control: Behavioral interventions that encourage the use of protective measures, such as bed nets and indoor residual spraying, can reduce vector-borne diseases like malaria and leishmaniasis.
Monitoring and Evaluation:
Assessing Impact: Regular monitoring and evaluation of behavioral interventions are essential to assess their impact and identify areas for improvement. This involves collecting data on behavior changes, infection rates, and community feedback.
Adapting Strategies: Based on evaluation results, strategies can be adapted and refined to enhance their effectiveness and sustainability.
Integrating Socioeconomic and Behavioral Approaches
Effective parasitology research and intervention programs must integrate socioeconomic and behavioral approaches. This holistic strategy ensures that interventions address both the underlying social determinants of health and the individual behaviors that contribute to the transmission of parasitic diseases.
Policy and Advocacy:
Health Equity: Advocating for policies that promote health equity and reduce socioeconomic disparities is crucial. This includes policies that ensure access to healthcare, improve living conditions, and provide education and employment opportunities.
Funding and Resources: Securing funding and resources for comprehensive parasitology programs that combine socioeconomic and behavioral interventions can enhance their reach and impact.
Collaboration and Partnerships:
Intersectoral Collaboration: Collaboration between health sectors, educational institutions, and community organizations is essential for addressing the multifaceted nature of parasitic diseases. Partnerships can leverage resources and expertise to implement comprehensive intervention programs.
Global and Local Partnerships: Engaging both global health organizations and local communities ensures that interventions are contextually relevant and globally informed.
Sustainability:
Long-Term Commitment: Sustainable interventions require long-term commitment and investment. This includes continuous funding, community involvement, and adaptive strategies to respond to changing conditions and emerging challenges.
Capacity Building: Building the capacity of local health systems and communities to manage parasitic diseases independently is key to sustaining health improvements.
In conclusion, behavioral and social research in parasitology is critical for understanding and addressing the complex interplay of factors that influence the prevalence and impact of parasitic diseases. By focusing on socioeconomic determinants and implementing effective behavioral interventions, we can make significant strides in reducing the burden of these diseases and improving health outcomes for vulnerable populations.
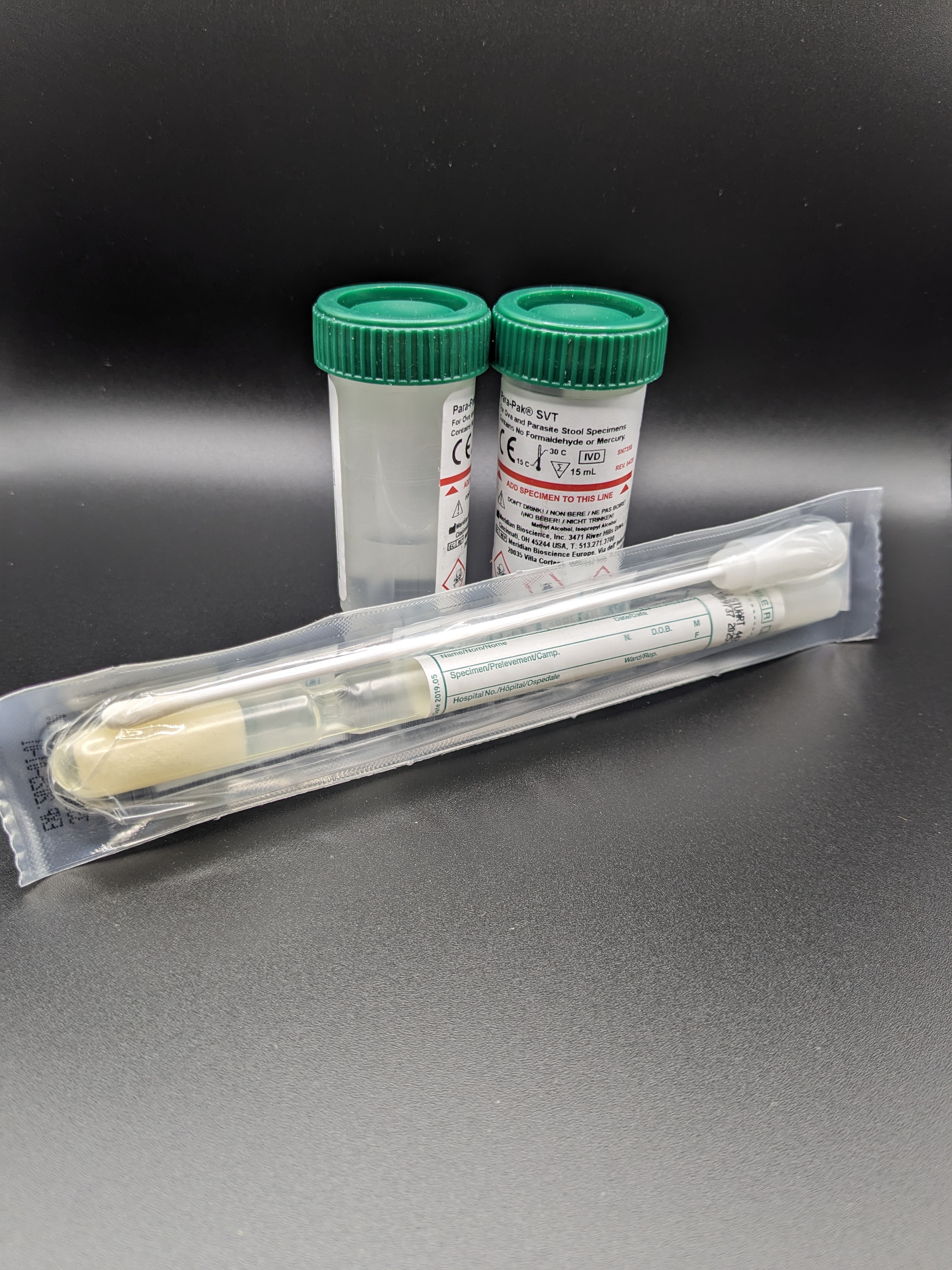
Discover What's Really Going On Inside Your Gut!
Experiencing stomach troubles? Our Full GI Panel Test can help! Identify bacteria, parasites, and fungi with state-of-the-art accuracy. Quick, non-invasive, and thoroughly analyzed by experts.
Take the first step towards better gastrointestinal health today!
Feel Refreshed and Balanced with Freedom Cleanse Restore!
Reset your digestive system and boost your overall well-being with our Freedom Cleanse Restore supplement. Designed to support detoxification, promote digestive health, and enhance nutrient absorption.
Reclaim your health—experience the benefits today!
Contact Information
11445 E. Via Linda, #2-419
Scottsdale, Arizona 85259 USA
1-480-767-2522
Hours: 7:30am to 4:00pm
Monday through Thursday.
Hours: 7:30am to 1:00pm on Friday.
Closed Saturday - Sunday.